Federal Drug Administration policy regarding blood donations from "men who have sex with other men":
http://www.fda.gov/biologicsbloodvaccines/bloodbloodproducts/questionsaboutblood/ucm108186.htm
What is FDA's policy on blood donations from men who have sex with other men?
Men who have had sex with other men (MSM), at any time since 1977 (the beginning of the AIDS epidemic in the United States) are currently deferred as blood donors. This is because MSM are, as a group, at increased risk for HIV, hepatitis B and certain other infections that can be transmitted by transfusion.
Why doesn't FDA allow men who have had sex with men to donate blood?
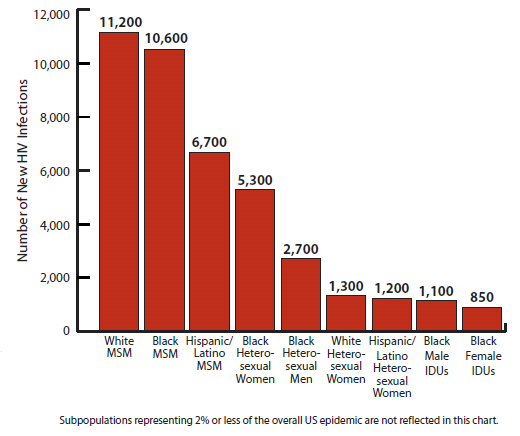
A history of male-to-male sex is associated with an increased risk for exposure to and transmission of certain infectious diseases, including HIV, the virus that causes AIDS. Men who have had sex with other men represent approximately 2% of the US population, yet are the population most severely affected by HIV. In 2010, MSM accounted for at least 61% of all new HIV infections in the U.S. and an estimated 77% of diagnosed HIV infections among males were attributed to male-to-male sexual contact. Between 2008 and 2010, the estimated overall incidence of HIV was stable in the U.S. However the incidence in MSM increased 12%, while it decreased in other populations. The largest increase was a 22% increase in MSM aged 13 to 24 years. Since younger individuals are more likely to donate blood, the implications of this increase in incidence need to be further evaluated.
Is FDA's policy of excluding MSM blood donors discriminatory?
FDA's deferral policy is based on the documented increased risk of certain transfusion transmissible infections, such as HIV, associated with male-to-male sex and is not based on any judgment concerning the donor's sexual orientation.
What about men who have had a low number of partners, practice safe sex, or who are currently in monogamous relationships?
Having had a low number of partners is known to decrease the risk of HIV infection. However, to date, no donor eligibility questions have been shown to reliably identify a subset of MSM (e.g., based on monogamy or safe sexual practices) who do not still have a substantially increased rate of HIV infection compared to the general population or currently accepted blood donors. In the future, improved questionnaires may be helpful to better select safe donors, but this cannot be assumed without evidence.
Isn't the HIV test accurate enough to identify all HIV positive blood donors?
HIV tests currently in use are highly accurate, but still cannot detect HIV 100% of the time. It is estimated that the HIV risk from a unit of blood has been reduced to about 1 per 2 million in the USA, almost exclusively from so called "window period" donations. The "window period" exists very early after infection, where even current HIV testing methods cannot detect all infections. During this time, a person is infected with HIV, but may not have enough virus or have developed sufficient antibodies to be detected by available tests. For this reason, a person could test negative, even when they are actually HIV positive and infectious. Therefore, blood donors are not only tested but are also asked questions about behaviors that increase their risk of HIV infection.
Collection of blood from persons with an increased risk of HIV infection also presents an added risk to transfusion recipients due to the possibility that blood that has already been collected and is being stored in a blood bank may be accidentally given to a patient in error either before testing is completed or following a positive test. Such medical errors occur extremely rarely, but given that there are about 17 million Whole Blood and red blood cell donations collected each year in the USA, they can occur.
Log in to comment